Baby Meadow’s Story: How Specialized NICU Care Saved One Preemie’s Life
At 37 years old, Elizabeth Hewett was both excited and nervous when she found out she was pregnant for the first time in April of 2022. She and her husband, Juan Cardona, had always wanted a child, so although it was slightly unexpected, the news of a baby brought joy.
For months, Elizabeth’s pregnancy was smooth and uneventful – everything was on track. Still, she was being monitored closely by Maternal-Fetal Medicine specialist Dr. James Hill due to her age, which made her pregnancy clinically high-risk. At an appointment on September 8, 2022, Dr. Hill was concerned about the lack of movement he observed, and he told Elizabeth that he would like her to go to CHRISTUS Children’s for further monitoring of the baby girl.
An Extended Stay
“The original plan was to monitor her for 24 hours and then send me home,” Elizabeth said. “But I ended up never leaving until after she was born.”
At CHRISTUS Children’s, Elizabeth’s blood pressure was dangerously high, and doctors were unable to stabilize it. Additionally, they also noticed the baby was not moving as she should, and they shared with Elizabeth that her baby was measuring at less than 1 percentile for her expected growth.
“They didn’t feel comfortable sending me home at that point,” Elizabeth said. “I was going into my 31st week of pregnancy and by then they were saying their goal was to just get me to 32 weeks.”
Time to Deliver
By September 15, her specialists began to note dips in the fetal heart rate and that she may be in distress. The next day, the baby had two significant dips within an hour.
“The doctors came in and explained that there was very little value for her gestationally since she wasn’t growing and that due to her lack of movement and the episodes with her heart rate, it was safest to not wait any longer to deliver,” Elizabeth said.
It was September 16, and Juan, who travels out of the country frequently for his job, wasn’t scheduled to be back until the following day.
“I wanted to wait but I knew we couldn’t,” Elizabeth said. “Luckily, my mom was able to come and be there with me for the delivery.”
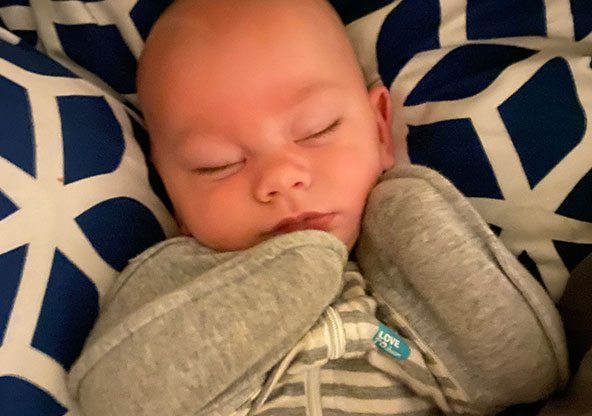
A few hours later, Meadow Cardona was born at 2:18 p.m., weighing just 2 pounds, 6 ounces.
“She had to be taken to the NICU immediately, which was hard, but I was relieved to know that my mom was with her,” Elizabeth said.
Later that evening, Elizabeth was finally able to meet her baby girl. And Juan, after rushing to get home as fast as he could, arrived at around 10 p.m. to see his wife and meet his daughter.
Further Challenges to Overcome
But the following weeks presented more challenges. Elizabeth ended up testing positive for COVID-19 and couldn’t visit Meadow for 10 days after that first meeting. Meadow was also receiving around-the-clock care, which is common for babies born prematurely, as their lungs and other organs are not developed enough, and they often struggle with a host of complications for the first few months of their lives.
Still, Elizabeth was thankful that both she and her daughter were at CHRISTUS Children’s. Meadow was under the care of Dr. Maria Pierce, a board-certified Perinatal-Neonatal physician, who kept Elizabeth informed of her daughter’s conditions, including both her struggles and her triumphs.
“It was so hard, but Dr. Pierce was really great,” Elizabeth said. “She would always call and keep us updated on everything that was going on. I knew she was taking the best care of our baby.”
The Highest Level of Care
CHRISTUS Children’s has a Level IV NICU, which is the highest level of care available for babies born as prematurely as Meadow. Since premature babies often have complex and varying needs, a high level of care with different specialists and experts available within the same facility leads to better outcomes for tiny preemies.
“Every newborn deserves the best possible start in life, and for babies who are born as prematurely as Meadow, specialized care like the kind we have in our Level IV NICU is critically important for both survival and long-term health,” Dr. Pierce said. “We are proud to provide the highest level of expertise and the necessary resources to give babies the greatest chance for a healthy future.”
Meadow endured many of the common conditions associated with extremely premature babies, including jaundice, feeding problems, issues with weight gain, and controlling her blood sugar. She experienced episodes of bloody stools which raised concern she had necrotizing enterocolitis—a life-threatening intestinal condition that can occur in premature babies because their fragile intestines are prone to breakdown—however, she was ultimately diagnosed with a cow’s milk allergy. In addition, she developed bilateral inguinal hernias and has a heart murmur from an atrial septal defect, which is still closely monitored.
Meadow spent 102 days in the NICU, receiving specialized care as she slowly grew bigger and stronger.
During that time, Elizabeth was grateful that she was able to stay in the Ronald McDonald House, located inside the hospital, so she never had to be too far from her baby’s side. The Ronald McDonald House Charities of San Antonio has 16 rooms inside CHRISTUS Children’s, just steps away from the NICU. Their mission is to provide a safe and supportive environment for families who are away from home while receiving essential medical services at Children’s.
Baby Meadow Now
Today, Meadow is home, but the family still travels regularly to CHRISTUS Children’s for follow-up appointments and care. In February, she had surgery to repair her hernias, and like many premature babies, she will continue to receive ongoing monitoring and care for many of her conditions, with regular appointments with her gastroenterology specialist, cardiologist, and endocrinologist.
“We come to Children’s all the time now, and we couldn’t be happier with the care we receive here,” Elizabeth said. “All of the nurses are great and the doctors are just wonderful. They always make sure to explain things in a way we can understand, and they never made us feel silly for asking questions. Being in the NICU was such a difficult and stressful time, but the team at Children’s really made it bearable.”